CRT-P vs CRT-D: A Detailed Guide to Understanding the Difference
Introduction: The Symphony of the Heart
CRT-P vs CRT-D: A Detailed Guide to Understanding the Difference by Dr. Kuntal Bhattacharya, Sr. Consultant Interventional Cardiologist, Kolkata
Dear friends and valued patients, I am Dr. Kuntal Bhattacharya, and for many years, my mission in Kolkata has been to help hearts beat stronger, longer, and more efficiently.
The human heart is perhaps the most incredible machine in existence. It’s a relentless, tireless pump, dedicated to sustaining life. Ideally, the four chambers of the heart—the two upper atria and the two lower ventricles—should contract in perfect, synchronized harmony, like a magnificent orchestra playing a beautiful symphony.
But what happens when the heart’s rhythm gets out of sync? What happens when the left ventricle, the main pumping chamber, starts contracting inefficiently, leading to a condition known as Heart Failure?
This is where the transformative power of modern cardiology comes in, specifically through a treatment called Cardiac Resynchronization Therapy, or CRT.
If you or a loved one has been diagnosed with heart failure, you’ve likely heard terms like CRT-P and CRT-D. These names can sound confusing, technical, and frankly, a little scary. My goal today is to demystify these devices, to translate the complex medical jargon into simple, human terms, and to explain the crucial difference between a CRT-P and a CRT-D.
Understanding this difference is not just about knowing two acronyms; it’s about understanding a life-changing decision in your journey toward a healthier heart. It’s about knowing whether your heart needs a conductor, or a conductor and a guardian angel. The right choice is pivotal to your health, safety, and long-term quality of life.
Section 1: The Heart of the Problem – Understanding Ventricular Dyssynchrony
To appreciate what CRT-P and CRT-D do, we must first understand the root problem: Heart Failure (HF).
Heart failure doesn’t mean the heart has “failed” or stopped; it means the heart muscle is weakened and cannot pump enough blood to meet the body’s needs. One of the most common causes of this weakening is an electrical timing issue, specifically in the left ventricle.
Imagine a water balloon that needs to be squeezed to push the water out. If you squeeze it evenly with both hands, the water jets out effectively. Now, imagine if one hand squeezes a fraction of a second before the other—the balloon doesn’t compress optimally, and the water output is weak and inefficient. This is what happens when the right and left sides of the heart, the two ventricles, don’t contract at the same time.
In a healthy heart, the electrical signal travels rapidly and synchronously. In many heart failure patients, particularly those with a Left Bundle Branch Block (LBBB), the electrical signal that tells the left ventricle to contract arrives late. This delay causes the walls of the left ventricle to contract in a disorganized, “wobbling” pattern—a phenomenon we call Ventricular Dyssynchrony.
The result? The heart struggles, symptoms like breathlessness and fatigue worsen, and the patient’s quality of life diminishes. The ongoing, inefficient contraction not only reduces the volume of blood pumped but also further stretches and damages the heart muscle over time, leading to a vicious cycle of decline. This is precisely the issue Cardiac Resynchronization Therapy (CRT) is designed to fix. It is a proactive intervention to interrupt this cycle and restore mechanical efficiency.
Section 2: The Core Concept – What is Cardiac Resynchronization Therapy (CRT)?
Cardiac Resynchronization Therapy is a revolutionary treatment for select patients with chronic, symptomatic heart failure, particularly those who have not responded adequately to optimal medical therapy alone. Its mission, as the name suggests, is to resynchronize the heart’s pumping action.
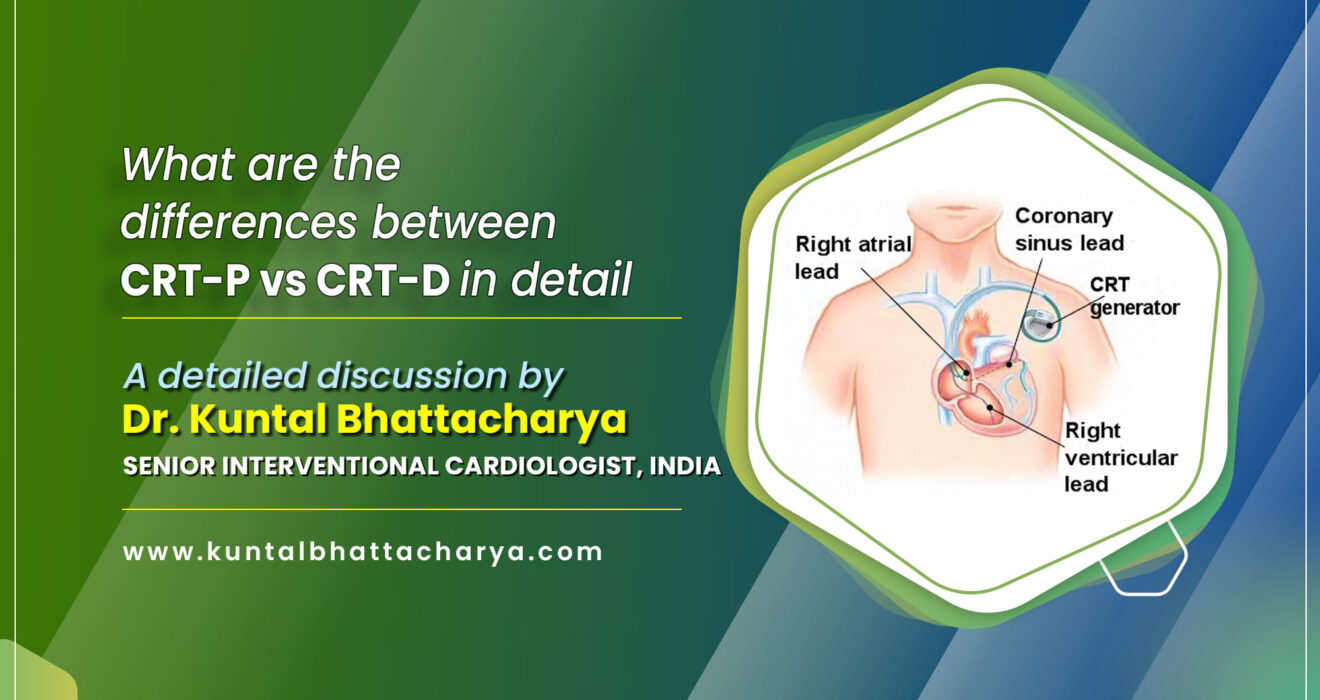
In simple terms, a CRT device is a highly specialized type of pacemaker. It is sometimes referred to as a Biventricular Pacemaker because it paces both the right and left ventricles. Unlike a standard pacemaker, which usually has one or two wires (leads) and only focuses on correcting a slow heart rate (bradycardia), a CRT device requires three leads:
- Right Atrium (RA) Lead (Optional): Used to monitor the natural electrical rhythm starting in the upper chambers.
- Right Ventricle (RV) Lead: To pace the right side of the heart, typically at the tip of the right ventricle.
- Left Ventricle (LV) Lead (The Crucial Third Lead): This lead is the defining feature. It is delicately placed, usually via a specialized procedure through the coronary sinus (a vein on the outside of the heart), to reach the surface of the left ventricle.
The magic of CRT lies in this third lead. By sending tiny, precisely timed electrical pulses to both the right ventricle and the left ventricle simultaneously (or nearly simultaneously with a programmed offset), the device effectively bypasses the native electrical block (LBBB) and forces the two chambers to contract at the same time.
It’s like hiring a conductor to bring the out-of-sync orchestra back into perfect rhythm.
The benefits of successful CRT are profound and well-documented in major clinical trials:
- Improved Ejection Fraction (EF): For many patients, the heart’s pumping efficiency increases significantly—sometimes by as much as 10-15 percentage points. This is known as “reverse remodeling.”
- Reduced Heart Failure Symptoms: Patients often report a dramatic decrease in fatigue and breathlessness, leading to an improvement in their NYHA (New York Heart Association) Functional Class.
- Better Quality of Life: Patients can walk farther, manage daily activities more easily, and regain independence.
- Reduced Hospitalizations: The therapy stabilizes the patient’s condition, leading to fewer unplanned visits and stays in the hospital for heart failure exacerbations.
- Improved Survival: CRT has been shown in studies to improve long-term prognosis for appropriate patient populations.
Now that we understand the core therapy, we can focus on the two options: CRT-P and CRT-D. The common part is the CRT—the resynchronization therapy. The difference lies in the suffix: Pacing versus Defibrillation.
Section 3: The Conductor – CRT-P (Cardiac Resynchronization Therapy-Pacing)
The CRT-P is the more focused of the two devices. The ‘P’ stands unequivocally for Pacing.
What the CRT-P Does
A CRT-P is essentially a powerful, sophisticated, triple-chamber pacemaker whose sole, singular focus is to deliver the resynchronization pacing.
- The Mechanism: It sends the precisely timed, low-energy electrical pulses through its three leads to the right and left ventricles, ensuring they squeeze together for optimal blood flow. It corrects the electrical timing issue, which in turn fixes the mechanical pumping issue.
- The Primary Goal: To treat the mechanical problem of dyssynchrony. Its job is to enhance the heart’s efficiency, improve symptoms, and reverse the structural weakening of the heart muscle over time. It is a therapeutic device aimed at structural and symptomatic improvement.
Who is a Candidate for CRT-P?
The decision to implant a CRT-P is based on strict international and national guidelines, which I meticulously follow here in Kolkata. Generally, a patient is considered for a CRT-P if they meet the criteria for CRT and, crucially, do not have a high enough risk profile for Sudden Cardiac Death (SCD) to warrant a defibrillator.
Typical criteria include:
- Chronic Heart Failure: Moderate to severe symptoms (NYHA Class II, III, or IV Ambulatory) despite maximum medical therapy.
- Severely Weakened Heart Muscle (Low Ejection Fraction – LVEF): The heart’s pumping capacity is significantly reduced, often defined as less than 35%.
- Significant Electrical Conduction Delay (Wide QRS Complex): An ECG shows clear evidence of dyssynchrony, typically measured by a QRS duration greater than 150 ms (milliseconds), or sometimes 130-149 ms with specific LBBB morphology.
- No Indication for ICD: The patient is not at high risk for life-threatening ventricular arrhythmias based on their Ejection Fraction, history, or other clinical markers. The patient needs the synchronization benefit but is considered relatively safe from sudden electrical catastrophe.
- Co-morbidities: Sometimes chosen for patients with multiple serious non-cardiac conditions where maximizing comfort and minimizing the risk of high-energy shocks is prioritized over aggressive SCD prevention.
Advantages of CRT-P
- Smaller and Lighter: The device is generally more compact as it does not require the large, high-voltage capacitor necessary for defibrillation.
- Longer Battery Life: Because the device is not constantly charging a high-energy capacitor for defibrillation shocks, the battery life often lasts longer (potentially 8-12 years or more), meaning fewer replacement procedures for the patient.
- Lower Initial Cost: The technology is less complex and therefore typically less expensive than the ‘D’ option, making it an accessible option where cost is a major consideration.
- Avoids Unnecessary Shocks: The patient is completely spared the risk of receiving an inappropriate high-energy shock, which can be a traumatic experience.
In essence, the CRT-P is a dedicated therapist and trainer for the heart, diligently working every second to restore efficient pumping, without the added responsibility of immediate cardiac rescue.
Section 4: The Guardian Angel – CRT-D (Cardiac Resynchronization Therapy-Defibrillator)
The CRT-D is often called a “combination device” because it provides both Cardiac Resynchronization Therapy and a second, life-saving function: Defibrillation.
If the CRT-P is the conductor, the CRT-D is the conductor plus a dedicated, on-board paramedic ready to intervene instantly.
What the CRT-D Does
The CRT-D performs the exact same functions as the CRT-P: it has the three leads, provides the biventricular pacing, and offers the perfect, synchronized rhythm to improve the heart’s function and the patient’s quality of life.
BUT, it also contains a powerful, specialized capacitor, a complex battery system, and advanced circuitry, which allows it to function as an Implantable Cardioverter-Defibrillator (ICD).
- The Mechanism:
- Pacing: Identical to CRT-P (resynchronization).
- Defibrillation: This device constantly monitors the heart’s electrical activity, listening hundreds of times a second. If it detects a life-threatening, chaotic, and ultra-rapid rhythm—like Ventricular Tachycardia (VT) or the deadly Ventricular Fibrillation (VF)—it immediately initiates its rescue protocol:
- It may first attempt Anti-Tachycardia Pacing (ATP), which is a rapid burst of pacing pulses to painlessly interrupt the rhythm.
- If ATP fails or the rhythm is VF, it instantly charges up and delivers a powerful, high-energy electrical shock directly to the heart muscle.
- The Primary Goal: To prevent Sudden Cardiac Death (SCD). SCD is often the result of VT/VF, where the heart muscle is essentially just quivering and cannot pump blood, leading to immediate collapse and death if not treated. The shock from the CRT-D acts as an electrical “reset button,” stopping the chaotic rhythm and allowing the heart’s natural pacemaker to resume a normal, life-sustaining rhythm.
The Risk of Sudden Cardiac Death (SCD)
Why is the defibrillator function necessary for some patients?
Patients with very weak hearts (extremely low LVEF, particularly less than 30-35%) are at a significantly higher risk of developing these lethal, disorganized rhythms, even if their heart failure symptoms are not severe. The damaged or scarred heart tissue (often from a previous heart attack) acts like a short-circuit, leading to electrical instability—a condition known as malignant arrhythmia.
For these patients, an SCD event can happen suddenly, without warning, and outside of a hospital setting. The presence of the CRT-D becomes an absolute necessity, acting as an internal safety net, ready to save the patient’s life within seconds—a speed no external emergency service can match. This is often called Primary Prevention (preventing a first event) or Secondary Prevention (preventing a recurrence after an event).
Who is a Candidate for CRT-D?
The primary indication for choosing CRT-D over CRT-P is the risk assessment for SCD.
A patient who needs CRT and has a high risk of SCD will be recommended for a CRT-D. This risk is typically determined by:
- Very Low Ejection Fraction (LVEF): Usually at or below 35%, even after being on optimal medical therapy for months, indicating a high inherent risk of fatal arrhythmias.
- Prior History of Life-Threatening Arrhythmias (Secondary Prevention): A documented history of surviving Ventricular Fibrillation or unstable Ventricular Tachycardia.
- High-Risk Patient Profile (Primary Prevention): Specific conditions like certain genetic syndromes (e.g., Long QT Syndrome) or extensive scarring of the heart muscle.
Considerations with CRT-D
While the life-saving potential is undeniable, there are trade-offs that we discuss openly:
- Bulkier Device: The housing is noticeably larger to accommodate the high-voltage capacitor.
- Shorter Battery Life: The constant need to be ‘ready’ for a shock and the periodic charging cycles drain the battery faster, often leading to replacement procedures sooner (typically 5-7 years).
- Risk of Shocks: The patient must be prepared for the possibility of receiving a shock. While life-saving shocks are necessary, there is a small risk of inappropriate shocks (when the device misidentifies a harmless, fast rhythm as a dangerous one). This is physically painful and mentally distressing, though modern devices have increasingly advanced algorithms to minimize this.
Section 5: CRT-P vs CRT-D: A Head-to-Head Comparison
The table below offers a simple, structured look at the key differences between the two devices. This is the heart of the matter—understanding the core functional distinction.
| Feature | CRT-P (Pacing) | CRT-D (Defibrillator) |
| Primary Function | Cardiac Resynchronization Pacing | CRT Pacing AND Defibrillation/Cardioversion |
| Primary Goal | Improve symptoms, heart function, and quality of life. | Prevent Sudden Cardiac Death (SCD) and improve heart function. |
| SCD Risk Profile | Low/Moderate risk of life-threatening arrhythmias. | High risk of life-threatening arrhythmias (VT/VF). |
| Electrical Output | Low-energy electrical pulses (pacing). | Low-energy pulses (pacing) AND High-energy electrical shocks (defibrillation). |
| Device Size | Slightly smaller and lighter. | Larger (due to the high-voltage capacitor). |
| Battery Life (Average) | Longer (8-12+ years). | Shorter (5-7 years). |
| Cost | Less expensive initially. | More expensive initially (due to advanced technology). |
| Patient Experience | Typically unnoticed, no risk of high-energy shocks. | Risk of receiving a shock (life-saving or inappropriate). |
Section 6: The Deciding Factor (CRT-P vs CRT-D)
This is the most critical section. In cardiology, there is no “one-size-fits-all” solution. The decision between a CRT-P and a CRT-D is not made by a machine; it is made by a cardiologist, based on a meticulous review of your individual health profile, in consultation with you.
When you sit down with me in my Kolkata clinic to discuss your Heart Failure treatment, we look at several key parameters to make the right recommendation. We follow a principle of balancing life prolongation (SCD prevention) with quality of life (symptom relief and shock avoidance).
1. The Ejection Fraction (LVEF) is Key
Your LVEF, or Left Ventricular Ejection Fraction, is the single most important metric. It is the percentage of blood pumped out of the heart’s main chamber with each beat.
- The ICD Threshold: Current guidelines strongly recommend an ICD (and thus a CRT-D) for nearly all patients with significant symptoms (NYHA Class II or III) and an LVEF of 35% or less, provided they are expected to live at least a year. If your LVEF falls into this high-risk zone, the primary mandate is safety, making the CRT-D the standard of care. We choose the guardian angel because the danger is high.
- The Borderline Zone: If your LVEF is slightly better (e.g., 35-40%), or if your SCD risk is low due to a different underlying cause of heart failure, we may discuss the option of a CRT-P, focusing purely on improving the mechanical pumping.
2. Co-Morbidities and Life Expectancy
We must also consider the bigger picture—a concept known as shared decision-making. If a patient has multiple other serious illnesses (e.g., advanced cancer, severe lung disease) and a limited life expectancy for reasons unrelated to heart failure, the added complexity, risk, cost, and potential side effects of a defibrillator (the shocks) might outweigh the potential benefit. In these compassionate care scenarios, a CRT-P might be favored to maximize comfort and quality of life, focusing exclusively on symptom relief. The goal shifts from maximum longevity to maximum comfort.
3. The Psychological Impact and Patient Preference
The prospect of receiving a shock, even a life-saving one, can be psychologically challenging, leading to anxiety and a reduced quality of life. We discuss this openly. While rare, inappropriate shocks are traumatic. For some patients, the guarantee of avoiding a high-energy shock (CRT-P) is a significant factor, provided their clinical risk profile allows for it, or if their risk is considered lower than the psychological burden of carrying a ‘shocking’ device.
The Humble Approach to Implantation:
Choosing between the P and the D is a shared journey. It involves a detailed discussion about risks, benefits, costs, and quality of life. My role is to present the evidence and the guidelines, but your feelings, concerns, and goals for your life matter most.
We analyze the electrical instability (the risk of sudden death) versus the mechanical failure (the need for better pumping).
- CRT-P: When the heart needs primarily better function and the electrical risk is manageable.
- CRT-D: When the heart needs better function AND immediate, instant protection from a potentially fatal electrical crisis.
Conclusion: Making the Best Choice for Your Heart (CRT-P vs CRT-D)
Heart failure is a chronic condition, but it is manageable, and with modern technology like Cardiac Resynchronization Therapy, the future is brighter than ever before. For many heart failure patients in Kolkata and across the world, the right CRT device offers a path back to a more active, independent life.
Whether you require a CRT-P (the dedicated conductor, optimizing the pump) or a CRT-D (the conductor with a guardian angel, providing optimal pump function plus life-saving protection), both devices represent the cutting edge of cardiac care. They are powerful tools designed to restore your heart’s rhythm and rejuvenate your quality of life.
The decision is sophisticated, intensely personal, and based on the latest science and a deep understanding of your unique heart condition.
If you are facing this decision, or if a previous evaluation suggested the need for a CRT device, I urge you not to navigate this complex path alone. As a Sr. Consultant Interventional Cardiologist committed to serving the people of Kolkata, I am here to provide the clarity, expertise, and personalized care you need to make the choice that is right for you.
A stronger heart, a clearer future, and a synchronized rhythm are within reach.
Ready to Discuss Your Heart’s Rhythm?
Consult Dr. Kuntal Bhattacharya to understand which Cardiac Resynchronization Therapy device—CRT-P or CRT-D—is the safest and most effective choice for your specific health needs.
Book Your consultation for details.
Disclaimer: This blog post provides general health information and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider like Dr. Kuntal Bhattacharya with any questions you may have regarding a medical condition.
Follow Dr. Kuntal Bhattacharya on Facebook & Youtube for regular updates.
Read Also:
- Exclusive Guide to Coronary Angioplasty: An essential Insight from Interventional Cardiologist (PCI)
- Treatment Areas for Advanced Cardiac Treatments in 2025
- How to Book an Appointment for Heart Specialist Doctor Dr. Kuntal Bhattacharya in Kolkata in 2025
- Modern Technology in Cardiac Devices in 2025
- Recovery and Care After CRT-P/D Implantation in 2025
- Leadless Pacemaker: Safe, Small, and Reliable Heart Solution
- How to Find the Best TAVI and TAVR Doctor in Kolkata in 2025?