Exclusive Guide to Coronary Angioplasty: An essential Insight from Interventional Cardiologist (PCI)
Introduction: The Lifeline Procedure for Your Heart
💻🩺 Exclusive Guide to Coronary Angioplasty: An essential Insight from Interventional Cardiologist (PCI) Dr. Kuntal Bhattacharya (Senior), Sr. Heart Specialist Doctor in Kolkata
As an Interventional Cardiologist, one of the most vital and life-saving procedures I perform is Coronary Angioplasty, often combined with stenting, which is collectively known as Percutaneous Coronary Intervention (PCI). If you or a loved one has been diagnosed with Coronary Artery Disease (CAD), understanding this minimally invasive treatment is crucial.
In simple terms, Coronary Angioplasty is a catheter-based procedure used to open blocked or narrowed coronary arteries—the very vessels that supply oxygen-rich blood to your heart muscle. Restoring this blood flow is critical, whether to relieve chronic chest pain (angina) or, more urgently, to save heart muscle during a heart attack (Myocardial Infarction).
Recognizing the Warning Signs: Possible Symptoms
Coronary Angioplasty is a treatment for Coronary Artery Disease (CAD). The symptoms that often lead to the need for this procedure are related to the heart muscle not receiving enough blood (ischemia). These symptoms can include:
- Angina (Chest Pain): This is the most common symptom. It can feel like pressure, tightness, squeezing, or aching in the chest. It often occurs with exertion and subsides with rest or medication (like nitroglycerin).
- Shortness of Breath (Dyspnea): Feeling breathless, particularly during activity or at rest in severe cases.
- Fatigue and Weakness: Unexplained or overwhelming tiredness, often a signal of reduced heart efficiency.
- Referred Pain: Discomfort that radiates to other parts of the upper body, such as the left arm, jaw, neck, back, or stomach.
- Symptoms of a Heart Attack (Emergency): Sudden, intense chest pain, cold sweat, nausea, dizziness, or lightheadedness. If you experience these, seek emergency medical care immediately.
Understanding the Root: Causes of Blockages
The underlying cause that necessitates a Coronary Angioplasty is almost always Atherosclerosis.
Atherosclerosis is a progressive disease where plaque—a sticky buildup of cholesterol, fat, calcium, and other substances—forms within the walls of your arteries.
As plaque accumulates, it narrows the artery, restricting blood flow (Stenosis). If the plaque ruptures, a blood clot can form, causing a sudden, total blockage, which leads to a heart attack.
Major Risk Factors for Atherosclerosis:
- High Blood Pressure (Hypertension)
- High Cholesterol (Dyslipidemia)
- Diabetes Mellitus
- Smoking (The single most preventable risk factor)
- Obesity and Sedentary Lifestyle
- Family History of heart disease
The Treatment Explained: Coronary Angioplasty (PCI)
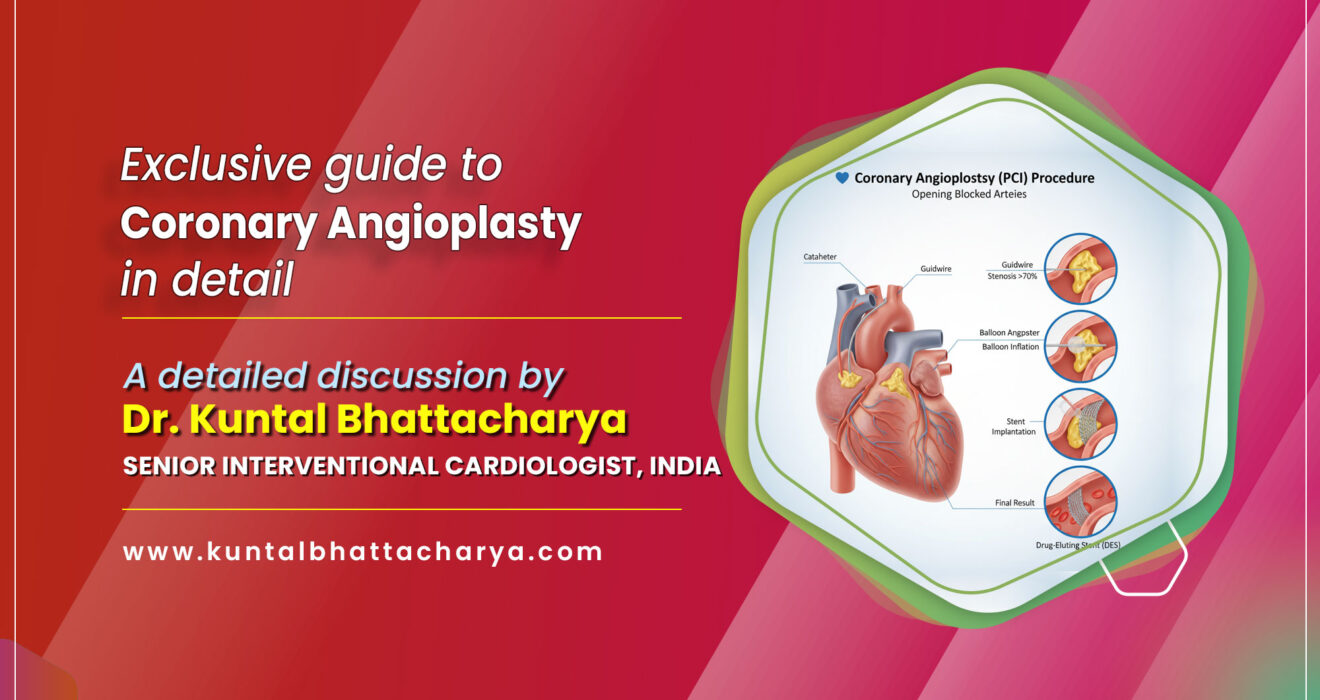
Coronary Angioplasty is a highly effective, minimally invasive treatment. Here is a step-by-step breakdown of the procedure and its different types.
The Procedure: How We Open the Artery
- Access: A thin, flexible tube called a catheter is inserted into an artery, usually in the wrist (Transradial approach, which is often preferred for faster recovery) or the groin (Transfemoral approach).
- Navigation: Using advanced X-ray imaging (Angiography) and a special contrast dye, I guide the catheter to the blocked coronary artery.
- Crossing the Blockage: A very fine guidewire is meticulously advanced across the blockage.
- Balloon Angioplasty: A catheter with a small, deflated balloon on its tip is threaded over the guidewire to the blocked site. The balloon is briefly inflated, compressing the plaque against the artery wall and widening the vessel.
- Stent Placement (The Standard Treatment): In the vast majority of cases, a stent—a tiny, expandable wire mesh tube—is permanently placed at the site of the blockage. The stent acts as a scaffold to keep the artery open and prevent it from collapsing or re-narrowing (restenosis).
Types of Percutaneous Coronary Intervention (PCI):
| Procedure Type | Description | Primary Goal |
| Balloon Angioplasty | Widening the artery using only an inflatable balloon. | Immediate opening of the vessel. Now rarely used without a stent. |
| Stent Implantation | Placing a metallic scaffold (stent) after ballooning. | Preventing restenosis (re-narrowing). |
| Drug-Eluting Stent (DES) | A stent coated with medication that slowly releases to prevent scar tissue formation, which significantly reduces the risk of restenosis. | This is the gold standard for most patients today. |
| Atherectomy | Using a rotating burr or laser on the catheter tip to shave away hard, calcified plaque before ballooning and stenting. | Treating heavily calcified or extremely tough blockages. |
When is Angioplasty the Right Choice?
The decision for a PCI is always tailored to the individual patient, but it is typically indicated when:
- You are experiencing a Heart Attack (STEMI or NSTEMI): This is an emergency life-saving procedure to restore blood flow immediately.
- You have severe or worsening Angina (chest pain): When medication and lifestyle changes are no longer effectively controlling your symptoms.
- Diagnostic Angiography reveals significant blockages: Blockages (typically $>70\%$) that put a large area of your heart muscle at risk.
Angioplasty vs. Bypass Surgery (CABG)
While PCI is a wonderful, minimally invasive option, it is not for everyone. In cases of very extensive disease, involvement of the main artery to the left side of the heart (Left Main Coronary Artery), or multiple complex blockages (especially in patients with diabetes), Coronary Artery Bypass Grafting (CABG) surgery may be the superior treatment, offering a more durable, complete revascularization. This is a crucial discussion I have with every patient.
A Final Word on Recovery and Life After PCI
Angioplasty is a remarkable procedure that has dramatically improved outcomes for countless patients. Recovery is typically fast—often a single overnight stay.
However, the procedure is only one step. The true success of PCI lies in your commitment to a heart-healthy future:
- Strict adherence to antiplatelet medication (e.g., Aspirin and a P2Y12 inhibitor) is non-negotiable to prevent blood clots in the stent.
- Lifestyle Modification: Adopting a low-fat, low-sodium diet, regular exercise, maintaining a healthy weight, and absolutely quitting smoking are essential.
- Regular Follow-up: Consistent monitoring with your Cardiologist is critical to managing all underlying risk factors.
By treating the blockage and embracing a healthier life, you can maximize the benefits of your Coronary Angioplasty and enjoy a vibrant, long future.
Next Step for Your Health
If you have persistent chest pain, shortness of breath, or multiple risk factors for heart disease, Always consult with a qualified cardiac specialist for diagnosis and treatment related to your personal health condition.
Disclaimer: This blog post is for educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition.
Follow Dr. Kuntal Bhattacharya on Facebook & Youtube for regular updates.
Read Also:
- Treatment Areas for Advanced Cardiac Treatments in 2025
- How to Book an Appointment for Heart Specialist Doctor Dr. Kuntal Bhattacharya in Kolkata in 2025
- Modern Technology in Cardiac Devices in 2025
- Recovery and Care After CRT-P/D Implantation in 2025
- Leadless Pacemaker: Safe, Small, and Reliable Heart Solution
- How to Find the Best TAVI and TAVR Doctor in Kolkata in 2025?
- Advanced Heart Treatments by Interventional Cardiologists in Kolkata